2025 Health Insurance Marketplace Plans: Best Value for Your Family

Understanding the complexities of 2025 Health Insurance Marketplace plans is essential for families seeking optimal coverage and financial security, requiring careful consideration of various factors to secure the most advantageous option.
Navigating the world of health insurance can often feel overwhelming, especially when trying to secure the best possible coverage for your loved ones. As we approach 2025, it’s more important than ever to understand the nuances of the options available. This guide will help you in comparing 2025 health insurance marketplace plans: identifying the best value for your family’s needs, ensuring you make an informed decision that protects both your health and your finances.
Understanding the 2025 Health Insurance Marketplace Landscape
The Health Insurance Marketplace, established by the Affordable Care Act (ACA), remains a crucial platform for individuals and families to find health coverage. For 2025, the marketplace continues to evolve, offering a range of plans designed to meet diverse needs and budgets. Understanding the fundamental structure and available subsidies is the first step toward making an informed choice.
The marketplace organizes plans into metal categories: Bronze, Silver, Gold, and Platinum. These categories indicate the percentage of healthcare costs the plan is expected to cover, not the quality of care. Bronze plans typically have lower monthly premiums but higher out-of-pocket costs, while Platinum plans have higher premiums but lower out-of-pocket expenses. Silver plans are particularly noteworthy as they may qualify individuals and families for extra savings, known as Cost-Sharing Reductions (CSRs), if their income falls within certain limits.
Key Changes and Continuities for 2025
- Continued Subsidies: Enhanced premium subsidies, initially boosted by the American Rescue Plan and extended by the Inflation Reduction Act, are expected to continue into 2025. These subsidies significantly lower monthly premium costs for many households.
- Increased Plan Options: Many states are seeing an increase in the number of participating insurers, leading to more plan choices and potentially more competitive pricing. This expanded competition can be beneficial for consumers seeking diverse options.
- Focus on Preventative Care: All marketplace plans are required to cover essential health benefits, including preventative care services, at no additional cost. This emphasis on early detection and prevention remains a cornerstone of ACA plans.
Before delving into specific plan types, it’s vital to assess your family’s unique healthcare needs and financial situation. This initial assessment will serve as a compass, guiding you through the myriad of choices and helping you pinpoint plans that truly offer value. The goal is to find a balance between affordable premiums and comprehensive coverage, ensuring your family is well-protected without unnecessary financial strain.
Decoding Plan Types: HMO, PPO, EPO, and POS
When exploring the 2025 Health Insurance Marketplace, you’ll encounter various plan types, each with its own structure regarding provider networks and referral requirements. Understanding these differences is crucial for choosing a plan that aligns with your family’s healthcare preferences and access needs.
HMOs, or Health Maintenance Organizations, typically have lower premiums and out-of-pocket costs but require you to choose a primary care physician (PCP) within their network. This PCP then refers you to specialists as needed. PPOs, or Preferred Provider Organizations, offer more flexibility, allowing you to see any doctor or specialist without a referral, both in and out of network, though out-of-network care usually comes at a higher cost.
Navigating Network Restrictions and Referrals
- HMO (Health Maintenance Organization): Generally lower premiums, but limited to a specific network of doctors and hospitals. You typically need a referral from your PCP to see a specialist.
- PPO (Preferred Provider Organization): Greater flexibility to choose doctors and hospitals, both in and out of network, without a referral. Out-of-network care costs more.
- EPO (Exclusive Provider Organization): Combines features of HMOs and PPOs. You don’t need a referral to see a specialist, but you are generally limited to doctors and hospitals within the plan’s network, except in emergencies.
- POS (Point of Service): A hybrid plan allowing you to choose between an HMO or PPO approach each time you need care. You’ll typically need a PCP referral for in-network care, but can go out-of-network for a higher cost.
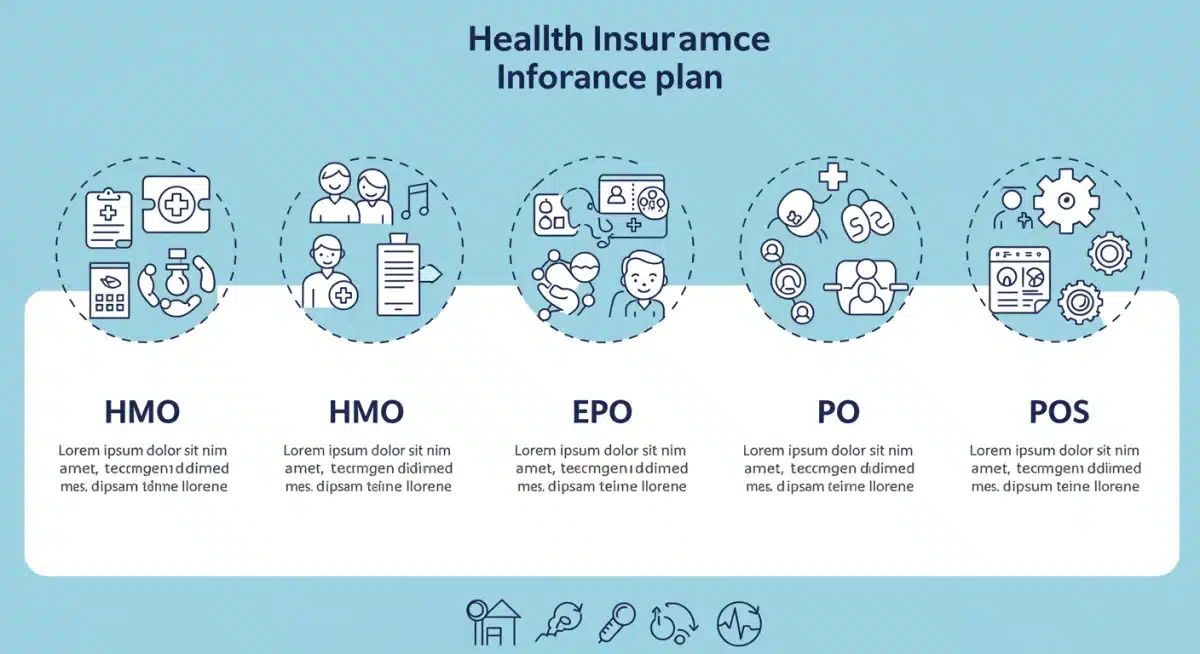
Understanding these distinctions is paramount, especially if your family has existing relationships with specific doctors or requires frequent specialist care. A plan that restricts your choice of providers could lead to unexpected out-of-pocket expenses or the need to change doctors, which can be a significant disruption. The goal is to match the plan type with your family’s established healthcare routines and anticipated needs for the upcoming year.
Assessing Your Family’s Healthcare Needs and Budget
Before diving into plan comparisons, a thorough assessment of your family’s healthcare needs and financial situation is essential. This step helps narrow down the options and ensures you select a plan that truly offers value without unnecessary costs or inadequate coverage.
Consider your family’s past medical history, current health conditions, and anticipated healthcare needs for 2025. Do you have young children who require frequent doctor visits? Are there any chronic conditions that necessitate regular specialist appointments or prescription medications? These factors will heavily influence the type of plan that provides the best value.
Key Considerations for Family Needs
- Current Health Status: Evaluate if anyone in your family has ongoing medical conditions, requires regular prescriptions, or anticipates significant medical procedures in the coming year.
- Provider Preferences: Do you have preferred doctors, specialists, or hospitals? Check if they are in-network for the plans you are considering.
- Anticipated Usage: Estimate how often your family will likely use healthcare services, including routine check-ups, specialist visits, and potential emergency care.
Your budget plays an equally critical role. Health insurance costs include not only the monthly premium but also deductibles, co-payments, co-insurance, and out-of-pocket maximums. A plan with a low premium might have a high deductible, meaning you pay more out-of-pocket before coverage kicks in. Conversely, a higher premium plan could offer lower out-of-pocket costs. It’s about finding the right balance that aligns with your financial comfort and risk tolerance.
Making Sense of Premiums, Deductibles, and Out-of-Pocket Maximums
Understanding the financial terminology associated with health insurance is fundamental to comparing 2025 health insurance marketplace plans effectively. Premiums, deductibles, co-payments, co-insurance, and out-of-pocket maximums all contribute to the total cost of your healthcare.
The premium is the fixed amount you pay every month for your health insurance coverage. It’s the most visible cost, but it’s only one piece of the financial puzzle. The deductible is the amount you must pay for covered healthcare services before your insurance plan starts to pay. For example, if your deductible is $5,000, you’ll pay the first $5,000 of covered services yourself.
Understanding Cost-Sharing Components
- Premiums: The monthly fee you pay to maintain your health insurance coverage. Lower premiums often mean higher deductibles and out-of-pocket costs.
- Deductibles: The amount you must pay for covered healthcare services before your insurance plan begins to pay. High-deductible plans often come with lower premiums.
- Co-payments (Co-pays): A fixed amount you pay for a covered healthcare service after you’ve paid your deductible. For instance, a $20 co-pay for a doctor’s visit.
- Co-insurance: Your share of the costs of a covered healthcare service, calculated as a percentage of the allowed amount for the service. For example, if your plan pays 80% of the cost, you pay 20%.
- Out-of-Pocket Maximum: The most you have to pay for covered services in a plan year. Once you reach this amount, your health plan pays 100% of the costs of covered benefits.
For families, especially those with anticipated high healthcare usage, a plan with a higher premium but lower deductible and out-of-pocket maximum might offer better overall value. Conversely, healthier families who anticipate minimal healthcare needs might find a high-deductible plan with a lower premium more cost-effective. It’s about weighing the upfront costs against potential future expenses.
Leveraging Subsidies and Financial Assistance
One of the most significant advantages of the Health Insurance Marketplace is the availability of financial assistance, primarily in the form of premium tax credits and Cost-Sharing Reductions (CSRs). These subsidies can significantly lower the cost of health insurance, making coverage more affordable for many families.
Premium tax credits, also known as subsidies, are based on your household income and family size. They can be used to lower your monthly premium payments. You can choose to have these credits paid directly to your insurance company each month, reducing your upfront costs, or you can claim them when you file your federal income tax return.
Maximizing Your Savings
- Premium Tax Credits: These credits are available to individuals and families whose income falls within certain percentages of the federal poverty level. They directly reduce your monthly premium.
- Cost-Sharing Reductions (CSRs): Available only with Silver plans, CSRs lower your out-of-pocket costs like deductibles, co-payments, and co-insurance. Eligibility is also based on income.
- Medicaid and CHIP: If your income is below a certain threshold, your family might qualify for Medicaid or the Children’s Health Insurance Program (CHIP), which offer low-cost or free health coverage.
It’s crucial to accurately report your estimated income for 2025 when applying through the marketplace, as this determines your eligibility and the amount of financial assistance you receive. Changes in income throughout the year should be reported to the marketplace to avoid discrepancies that could affect your subsidies. Leveraging these financial aids is key to identifying the best value plan, as they can dramatically alter the real cost of coverage for your family.
Tips for a Smooth Enrollment Process and Ongoing Management
Once you’ve identified potential plans that offer the best value for your family, the next step is a smooth enrollment process. This involves careful attention to detail and understanding key deadlines. Open enrollment typically runs for several weeks each fall, providing the primary opportunity to select or change your plan for the upcoming year.
Beyond initial enrollment, effectively managing your chosen plan throughout the year is equally important. This includes understanding your benefits, knowing how to access care, and keeping your marketplace information updated. Proactive management can prevent unexpected costs and ensure you maximize your plan’s benefits.
Ensuring a Seamless Experience
- Gather Necessary Documents: Have income statements, Social Security numbers, and current insurance policy information ready before you start the application.
- Utilize Marketplace Tools: The marketplace website offers comparison tools, calculators, and navigators who can provide free, unbiased assistance.
- Review Your Plan Annually: Even if you are satisfied with your current plan, market offerings change. Re-evaluate your options each open enrollment period to ensure you still have the best value.
Remember to update your marketplace account promptly if you experience any life changes, such as marriage, divorce, birth of a child, or significant income fluctuations. These events can impact your eligibility for subsidies or qualify you for a Special Enrollment Period (SEP), allowing you to change plans outside of open enrollment. Staying informed and proactive is the best way to ensure your family’s health insurance continues to meet their evolving needs and offers optimal value.
| Key Factor | Description for 2025 Planning |
|---|---|
| Plan Categories | Bronze, Silver, Gold, Platinum indicate cost-sharing levels; Silver plans offer Cost-Sharing Reductions. |
| Network Types | HMO, PPO, EPO, POS define provider access and referral requirements. Choose based on family needs. |
| Financial Aid | Premium tax credits and CSRs significantly reduce costs. Accurate income reporting is crucial for eligibility. |
| Enrollment & Management | Be aware of open enrollment periods, utilize marketplace tools, and update information for life changes. |
Frequently Asked Questions About 2025 Health Insurance
Metal categories (Bronze, Silver, Gold, Platinum) reflect how costs are split between you and your plan. Bronze plans have lower premiums but higher out-of-pocket costs, while Platinum plans have higher premiums and lower out-of-pocket costs. Silver plans offer unique cost-sharing reductions for eligible individuals.
Eligibility for premium tax credits and Cost-Sharing Reductions is based on your household income and family size relative to the Federal Poverty Level. You can check your eligibility by entering your estimated income and family details on the Health Insurance Marketplace website during the application process.
It depends on the plan type and your doctors’ network participation. HMOs and EPOs have more restricted networks, while PPOs offer more flexibility. Always verify that your preferred doctors and specialists are in-network for any plan you are considering before enrolling.
The out-of-pocket maximum is the most you’ll have to pay for covered healthcare services in a plan year. Once you reach this limit, your insurance plan pays 100% of additional covered costs. It’s crucial because it protects you from catastrophic medical expenses, providing a cap on your annual financial liability.
The primary time to enroll or change your plan is during the annual Open Enrollment Period, which typically occurs in the fall. However, certain life events like marriage, birth, or loss of other coverage can qualify you for a Special Enrollment Period (SEP) outside of this window.
Conclusion
Choosing the right health insurance plan for your family in 2025 requires a strategic approach, blending careful research with a clear understanding of your specific needs and financial situation. By thoroughly comparing the various options available on the Health Insurance Marketplace, understanding the different plan types, and leveraging available financial assistance, you can secure a plan that not only provides comprehensive coverage but also offers the best value. Remember that health insurance is a dynamic landscape; continuous monitoring and annual reassessment during open enrollment will ensure your family remains well-protected and financially secure for years to come.